Top 10 Major Challenges in Healthcare Industry and Their Solutions
The healthcare industry is grappling with a range of challenges that strain both resources and care delivery.
For instance, while there are pressures on earnings, the industry is also grappling with a tough situation in the capital markets, as Mckinsey’s analysis has revealed. There is a pressure on balance sheets and cash on hand is on the decline, as the trajectory from 2019 to 2023 shows.
At the same time, there’s no shortage of emerging solutions to help ease these burdens. Technology, particularly in the form of AI and data-driven tools, is offering new ways to reduce costs and improve operations.
Healthcare organizations prioritizing productivity improvement efforts within their core functions are poised to achieve significant savings. Likewise, those who fail to do so each year are likely to find themselves struggling to catch up. As McKinsey notes, these productivity gaps are becoming harder to ignore.
The savings expected from AI in healthcare is substantial. As McKinsey further states, AI technologies could generate $24 billion to $48 billion in annual savings for hospitals and $10 billion to $30 billion for physician groups by cutting administrative costs over the next five years.
The path forward is clear—leveraging technology to tackle long-standing inefficiencies could help healthcare providers stay afloat financially while improving patient care at the same time.
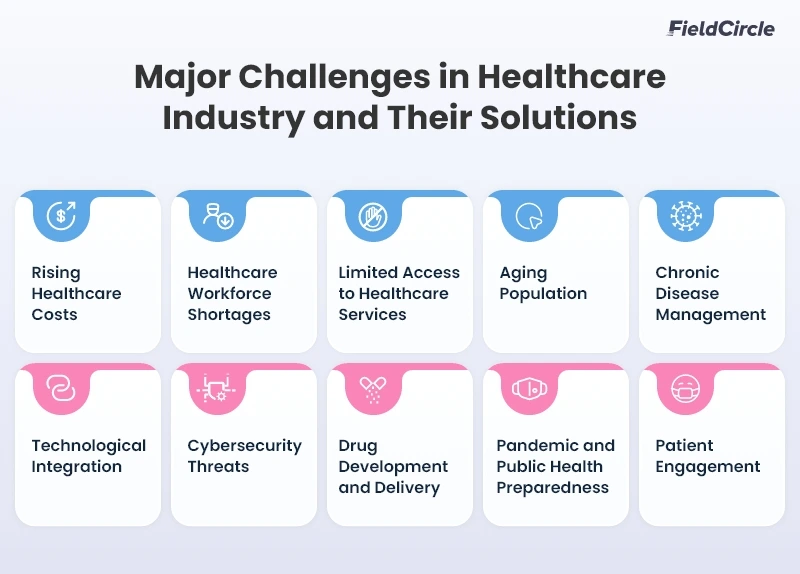
As we move ahead, we discuss the following 10 challenges facing healthcare businesses and the appropriate solutions to ace them.
- Rising Healthcare Costs
- Healthcare Workforce Shortages
- Limited Access to Healthcare Services
- Aging Population
- Chronic Disease Management
- Technological Integration
- Cybersecurity Threats
- Drug Development and Delivery
- Pandemic and Public Health Preparedness
- Patient Engagement
1. Rising Healthcare Costs
Inflation and affordability issues impact patients, providers, and insurers. Administrative expenses, insurance complexities, pharmaceutical pricing, and inefficiencies in hospital operations continue to drive up costs, making quality healthcare less accessible to many individuals. According to the National Health Expenditure Accounts (NHEA) reports, the U.S. healthcare spending was $4.9 trillion or $14,570 per person in 2023, making up 17.6% of the nation’s GDP. This marks a 7.5% year-over-year increase, leading to significant economic strain on households and businesses.
People without comprehensive insurance coverage experience high out-of-pocket costs that impact their healthcare. As a result, 21% of adults have not filled their prescriptions, and 61% skipped or postponed their needed care. Additionally, 41% have debt due to medical or dental bills. To make matters worse, the increasing hospital operational costs, including medical equipment maintenance and workforce salaries, further make the healthcare system costly for the general public.
One of the likely solutions to minimize healthcare costs includes implementing technology-driven financial planning, including predictive analytics for data-driven decision-making. With it, healthcare organizations can successfully optimize budgeting and resource allocation, preventing unnecessary expenses.
Potential tools to use include AI-powered billing software which minimizes administrative overhead, while automated medical coding minimizes errors and accelerates insurance approvals. Expanding telemedicine and preventive care programs reduce healthcare spending by lowering hospital admissions and emergency visits. Further, promoting value-based care models to incentivize healthcare providers for preventive care, wellness programs, and chronic disease management must be encouraged.
2. Healthcare Workforce Shortages
When healthcare staff is not enough, obviously, it directly affects patient care quality, healthcare accessibility, and eventually hospital efficiency. According to Mercer’s study, in 2025, there will be a shortage of over 400,000 home health aides and 29,400 nurse practitioners. Another report suggests that the U.S. healthcare workforce is projected to face a shortage of 100,000 medical professionals by 2028.
Increasing patient demand and early retirements are the primary causes of this workforce-related crisis. High demand for healthcare and healthcare services with finite medical professionals create longer wait times, reduced patient interactions, and higher workplace stress. Due to high workloads and insufficient support systems, hospitals struggle to retain healthcare workers, and as a result staffing shortages occur.
To mitigate these looming issues, hospitals should deploy workforce management software and optimize staff scheduling to ensure effective manpower allocation. The adoption of the software will assist in efficient workforce capacity planning and reduce burnout. The real-time tracking and AI-powered resource allocation features will aid in precise workforce distribution and there will be no disruption.
Another step to initiate is expanding telehealth services which will allow medical professionals to handle virtual consultations and lower the burden and stress of on-site staff. Last but not the least, healthcare facilities should invest in mental healthcare support programs to improve staff well-being and increase workforce retention.
3. Limited Access to Healthcare Services
Rural and underserved populations still continue to face issues when it comes to accessing healthcare services. The Health Resources and Services Administration (HRSA) report revealed that in 2022, 7.8% of US counties had no primary care physician, and the national ratio was 83.8 per 100,000 people. The lack of healthcare institutions and specialized medical professionals in remote areas limits patient care options. People in such places have to travel miles and miles for essential treatments. This contradicts the situation in cities where 24/7 medical care is on the go.
Likewise, financial barriers are also a significant hindrance to attaining proper healthcare. According to the CDC’s 2023 report, 6.4% of people over 18 failed to obtain medical care, and 87.8% went to unusual places for treatment due to cost constraints. Uninsured or underinsured patients delay preventive care, which leads to severe health complications and increased healthcare costs down the road.
One of the countermeasures to make healthcare accessible to more people is implementing community-based healthcare programs. Deploying trained medical staff to rural and underserved regions for real-time remote consultations makes medical care accessible, ensuring needy people receive the proper medical attention. In a way, it improves service management effectiveness.
Another way is to introduce subsidized healthcare plans which will help the low-income population access appropriate medical care, ensuring financial stability. Similarly, investing in virtual healthcare services helps improve the patient experience and that will reduce the gap between urban and remote care systems.
4. Aging Population
The growing aging population places immense pressure on healthcare systems. In the coming years, the need for specialized elderly care will be prominently high, demanding more time, effort, and resources for this demographic. By 2030, people aged 65 and older will comprise 20% of the US population. This means a rise in chronic illnesses, cognitive disorders, and mobility impairments, increasing the demand for specialized elderly care workers. This adds more pressure on hospitals, clinics, and long-term care facilities to cater their services to elderly people.
Increasing elderly people means more retirement, adversely impacting the healthcare sector and intensifying workforce shortages. The U.S. healthcare system is expected to face a deficit of 1.2 million registered nurses and 121,900 physicians, making it challenging to meet the medical needs of older adults. The problem of maintaining adequate staff degrades patient care quality and heightens hospital readmission rates.
Implementing preventive maintenance programs for elderly care equipment helps mitigate the systematic challenges posed by an aging population. Healthcare organizations must invest in healthcare maintenance management to keep senior patient care medical devices in optimal condition.
Correspondingly, AI-driven predictive analytics enables healthcare providers to anticipate age-related health risks, allowing for early intervention. Further, increasing the trend of home healthcare services reduces hospital dependency.
5. Chronic Disease Management
One of the biggest challenges for the healthcare industry, chronic diseases contribute to high mortality rates and increase the financial burden on patients and healthcare systems, making them. According to the CDC, 6 in 10 US adults are affected by a chronic disease, while 4 in 10 adults have multiple chronic conditions. To address this issue, the US government has allocated $1,559,414,000 in the FY 2025 budget for chronic disease prevention and health promotion.
However, conditions like diabetes, cardiovascular diseases, and respiratory disorders gradually develop over time, demand lifestyle modifications, and require ongoing medical treatment, which ultimately create a need for long-term medical costs. With a significant population of US adults suffering from chronic conditions, the challenge of handling extensive patient records cannot be neglected. In this effort, managing massive amounts of data increases the workload and stress for healthcare workers.
The potential solutions here are deploying IoT-enabled wearables that enables real-time health tracking and enhances chronic disease management. IoT comes with several benefits for healthcare facilities. The data-driven analytics facilitated by IoT allow monitoring of vital signs to detect early warning symptoms and adjust treatment plans accordingly. Further, integrating AI-driven analytics improves medication adherence and preventive care strategies to optimize personalized healthcare programs.
Substantial investment in public awareness campaigns about chronic disease prevention and remote patient monitoring is also a great step. It reduces incident rates and hospital readmissions and promotes better health outcomes while lowering long-term costs.
6. Technological Integration
As digital health technologies rapidly advance, healthcare providers struggle to keep up with new systems, software, and automation tools, making technology integration a major challenge for the healthcare sector. The digital health market is projected to reach $38 billion by 2025, an increase of $24.1 billion from its 2020 global valuation of $13.9 billion.
However, difficulty incorporating different Electronic Health Records (EHRs) and healthcare systems, expensive IoT devices and AI-powered solutions, and a lack of standardized systems obstruct effective technology adoption. Healthcare organizations still rely on outdated systems and lack proper tech infrastructure, which increases compatibility issues.
Employee resistance to new technology adoption, along with concerns about the trust, accuracy, and ethics of AI-driven healthcare solutions, further slow down digital transformation efforts.
The healthcare sector must implement interoperable EHRs for seamless data exchange between hospitals, clinics, and pharmacies. To streamline maintenance, it must integrate CMMS into its operational ecosystem. Further, preference should be given to cloud-based platforms to secure data and reduce risks associated with fragmented IT systems.
Hospitals should implement AI-driven automation to streamline workflow management and reduce administrative burdens. As a result, medical professionals will be able to dedicate themselves entirely to patient care. Similarly, healthcare facilities should train employees in new technologies and offer benefits to maximize productivity.
7. Cybersecurity Threats
As healthcare adopts advanced technology, the industry continues to face unprecedented cyber threats, which threaten patient data and hospital operations. In 2024, the average cost of a single healthcare data breach was $9.77 million, making it the most expensive industry for cyber attacks. Since 2011, healthcare has been the costliest sector for data breaches among critical infrastructure entities.
Ransomware attacks, phishing scams, and system vulnerabilities still compromise healthcare organizations and result in data loss, identity theft, and financial damage. In May 2024, UnitedHealth Group was attacked by ransomware, which affected around 190 million people. The company paid $22 million in bitcoin ransom to avoid the leak of patient information.
The healthcare sector must also comply with HIPAA and other data privacy laws. This need also makes securing large amounts of sensitive medical records challenging. As a result, many hospitals and clinics struggle to balance data accessibility with security measures, increasing their vulnerability to cyber threats.
To have robust digital security, healthcare organizations must adopt multi-layered cybersecurity frameworks to protect patient information. Implementing HIPAA-compliant encryption andd secure cloud storage solutions prevent data breaches and ensure compliance.
AI-driven threat detection systems should monitor cybersecurity for building management vulnerabilities in real time to prevent attacks before they happen. Staff training programs should also be introduced to educate employees on phishing prevention, secure password management, and incident response protocols to reduce human error in cybersecurity breaches.
8. Drug Development and Delivery
Issues in drug delivery causes treatment delays and higher costs. In 2023, healthcare facilities faced a quarterly shortage of 301 drugs, a 13% increase from the past year, marking the most drug shortage in the last 10 years. Such delays affect essential meds for cancer, chronic diseases, and infectious conditions.
In general, drug discovery and approval are incredibly lengthy and expensive. It is evident that the average cost of discovering and developing a drug is $2.8 billion. The process takes around a decade, and even after that, 90% of therapeutic molecules do not pass the Phase-II clinical trials and regulatory approval. Considering the success rate, expenses, and time required in the R&D of a drug, the availability of new life-saving medication in the market becomes extremely rare.
One way to increase drug delivery to market is to use AI-driven drug discovery platforms. These platforms accelerate clinical trials and approval by analyzing massive datasets to find promising drug candidates faster. They also predict molecular interactions, toxicity, and efficacy.
Blockchain-based tracking systems improve supply chain management by monitoring real-time drug production, storage, and distribution. Implementing automated inventory management helps hospitals and pharmaceuticals prevent shortages and deliver medications to patients on time. Regulatory agencies must also simplify the approval process through data-sharing models so that effective drugs can enter the market faster.
9. Pandemic and Public Health Preparedness
The COVID-19 pandemic exposed the vast gaps in public health emergency preparedness. It highlighted the need for better resource allocation, crisis management, and disease surveillance. According to a Trust for America’s Health report, the CDC’s Public Health Emergency Preparedness (PHEP) program, which oversees emergency preparedness, received annual funding of $735 million. This is $265 million short of the $1 billion recommended by the public health community.
Lack of emergency preparedness means delayed responses to outbreaks, inadequate PPE supplies, and overwhelmed hospitals during pandemic surges. Healthcare systems struggle with vaccine distribution, contact tracing, real-time disease monitoring, and prolonged health crises. Without enough funding, future pandemics will be even more dangerous to global health security. If something like COVID-19 occurs tomorrow, the same situation of panic, scarcity, and fear will prevail and take the world back to 2019.
Governments and healthcare organizations must adopt predictive analytics and AI-driven disease surveillance to respond to pandemics. These technologies will allow real-time tracking of emerging health threats and respond before outbreaks get out of hand.
And investment in medical supply chain resilience is key. Automated inventory management will ensure hospitals, clinics, and pharmacies have adequate stockpiles of critical medications, ventilators, and PPE. Strengthening public-private partnerships will also provide emergency funding for rapid vaccine development and distribution so the healthcare sector can respond quickly to future crises.
10. Patient Engagement
Low patient engagement is a significant obstacle to good health. If patients don’t follow their treatment plans, their health worsens, and costs increase. A study of 82,000 type 2 diabetes patients found that 63.6% had treatment changes, and 38.6% stopped medication due to a lack of engagement and support.
Patients struggle to understand their treatment plans, navigate the medical system, and get real-time health information. Poor communication between providers and patients makes it worse, resulting in missed appointments, non-compliance with meds, and preventable hospitalizations.
AI chatbots and mobile health apps boost patient engagement by giving personalized healthcare advice, medication reminders, and real-time communication with doctors. Patients take control of their health and improve treatment adherence and outcomes.
Telemedicine platforms improve doctor-patient communication, allowing virtual consultations, health monitoring, and treatment changes without in-person visits. Providers must also educate patients so they receive clear and simple information about their condition and treatment. Implementing personalized care plans and digital health coaching services further engages patients in their healthcare journey.
Conclusion
Healthcare maintenance comes with its share of challenges. To stay on top of things, organizations need reliable solutions to keep operations running smoothly.
FieldCircle’s healthcare maintenance software meets this need by providing healthcare teams with the right tools to manage tasks more efficiently. It offers a clear overview, and helps teams stay organized.
With FieldCircle, there are no roadblocks as issues are resolved before they snowball into major hurdles. Healthcare providers are thus able to deliver quality care in a smooth manner.
